Dec 13: Blog by Julia Drylewicz: How “playing it safe” may lead to increased mortality
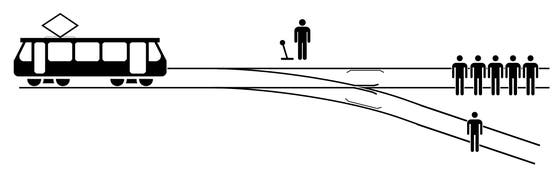
We all know the trolley dilemma in which a runaway trolley heads towards five people on a track. You have the option to divert the trolley onto another track where only one person stands, sacrificing that one individual to save the other five. With the recent approval of maternal vaccination against the respiratory syncytial virus (RSV) by both the European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA), this dilemma takes another meaning.
The approval of maternal vaccination against RSV will undoubtedly have an enormous public health impact, as RSV is the primary cause of death in children under 5. Remarkably, the EMA and the FDA made different recommendations for the time of vaccination during pregnancy. While the FDA decided to stay on the “safe” side by recommending vaccination relatively late during pregnancy (32-36 weeks), the EMA recommends vaccination between 24 and 36 weeks of pregnancy. The different recommendations are due to different interpretations of safety data of the clinical trial. The EMA concluded that there are no major safety concerns and decided that the vaccine can be safely administered relatively early during pregnancy. The FDA, on the other hand, stressed a small (albeit non-significant) increase in premature birth rates in the vaccinated group.
Within the Center for Translational Immunology, we are proud to have mathematical modelers in the Computational Immunology Core, investigating both basic immunology and the impact of interventions. We have developed a mathematical model to predict the potential impact of maternal vaccination against RSV. This model uses immunological knowledge such as time to reach antibody peak levels after vaccination, placental antibody transfer rates between the vaccinated mother and the child, and the distribution of gestational age at birth. Using this model, we studied the impact of the time of vaccination during pregnancy on the predicted number of RSV deaths or hospital admissions that could be prevented (or at least postponed) by such an intervention. We have recently updated our model based on the, now approved, vaccine and applied it to mortality data from low- and middle-income countries (LMICs) as those countries have the highest burden of RSV death (Willemsen et al. Vaccine:X, 2023). Following the different recommendations of the FDA and EMA, we wrote a commentary (Willemsen et al., Pediatric Infectious Disease Journal, 2023) reporting how those recommendations could impact the number of averted RSV cases in LMICs. Based on age-at-death data from LMICs, and looking at the extreme scenario of vaccination at 24 or 32 weeks of pregnancy, we estimated that, respectively, up to 94 and 82 percent of all RSV mortality cases could be prevented. Considering the estimated total number of RSV mortality cases among infants under 6 months in LMICs, maternal RSV vaccination has the potential to reduce yearly deaths by 3,300.
If we were to vaccinate only late during pregnancy, we may be avoiding a possibly increased risk of early birth but would fail to protect all preterm newborns who are most at risk for RSV infection. As in the trolley dilemma, with the FDA recommendations we may thus be saving the life of one at the cost of the lives of five others.
